Health Editor’s Note: Baby Boomers (people born from 1945–1965 are at least five times more likely to have hepatitis C than other adults. Hepatitis C is very insidious because you can be a carrier (have been infected) but do not show any symptoms. A specific reason for increased rates of Hepatitis C in the age group is not known but is probably due to the being alive during the 1960s through 1980s when transmission for this type of hepatitis was high.
People of this age group could have been infected from medical procedures or equipment before universal infection control procedures were put into place. Of course sharing needles for drug injection could have been a cause to be in contact with this type of hepatitis. Sharing just one contaminated needle could be the reason to develop hepatitis C. Others may have been infected from contaminated blood or blood products (plasma, factor for clotting for hemophiliacs, etc. before the screening (1992) began for this viral agent in the blood supply. Sometimes there may not be an obvious cause/reason/action to have contracted this disease.
Information from the CDC encourages every one in this age group to be tested. This would be a matter to discuss with your own healthcare provider. Essentially the blood test checks for antibodies (agents released into the blood stream when exposed to a disease that the body has recognized and has tried to stop) that your body would have developed if exposed to the virus. There are two results from the antibody test: 1) negative or non-reactive which means you do not have Hep C, unless you were recently exposed and your body has not had time to build up antibodies. If that is the case, you will have a subsequent test. 2) A positive or reactive result means that your body has been exposed to the Hep C virus at some period in time. A positive result does not mean you have Hep C but will confirm that you at some time were exposed to the virus. Of course a reactive test will require that you have an additional test to see if you now actively have Hep C.
Since so many VT readers fall into the Baby Boomer age group and are extra susceptible to contracting this disease, take a look at the nuts and bolts of Hepatitis C…….Carol
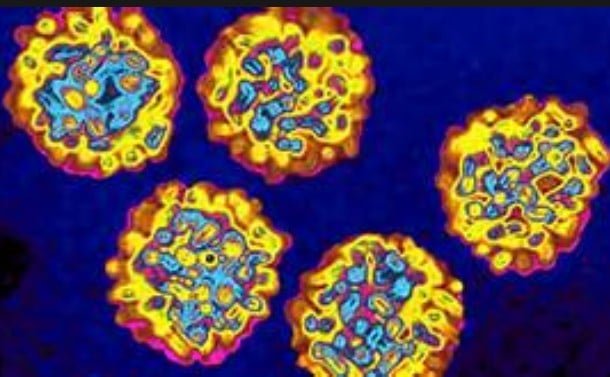
Becoming infected with hepatitis C virus (HCV) creates a disease of the liver which can lead to a chronic infection and is now the leading cause of liver illness. Vaccines against hepatitis A and hepatitis B exist, but there is no vaccine is available for this form of hepatitis. For those who develop chronic hepatitis C, the chance of developing cirrhosis of the liver is between 20 percent and 30 percent within 20 to 30 years. Acute HCV infections have become rarer, but still occur and will eventually produce a chronic infection in between 70 and 80 percent of those who do become infected with the hepatitis C virus.
While the United States has seen a decrease in cases of chronic HCV, up to 210 million people may be affected by HCV infection and HCV has become the leading cause of liver cancers in Europe. According to the CDC (U.S. Centers for Disease Control and Prevention), during the middle of the 1980s approximately 70 Americans out of every million of the population developed acute hepatitis C. There has been a 90 percent decrease in cases of acute hepatitis C between the years of 1994 and 2006 with about seven new cases per million.
How Can Someone be Infected with HCV?
Hepatitis C can be spread by blood to blood contact which in developed countries may be through blood transfusions of unscreened blood or blood products (clotting factors, platelets, immunoglobulin, plasma, and Rhogam), although due to vigorous screening measures, there has been no documented transfusion-related case of hepatitis C in the U.S. for over ten years.
Two other infection sources are shared needles during injected drug use or rarely through sexual exposure. Unlike the human immunodeficiency virus (HIV,) there must be opened sores (some sexually transmitted diseases (STDs) produce sores which can bleed) or the ability of blood products to be passed directly to another person’s blood supply during sexual activity. Before the screening process for hepatitis C virus, there were cases of hepatitis C infection in those who received organ donations from an infected person.
In developing countries the primary source of HCV infection is from unsterilized needles and inadequately screened blood and blood products but all the above mentioned conditions can also be a factor in the spread of HCV infection.
Occupational accidental blood exposure, due to blood spatter or accidental sticks from infected needles, can occur. Contact sports can also result in blood to blood exposure. Improperly sterilized dental and medical equipment may harbor the virus. Needles and injection equipment, hemodialysis equipment, jet air guns, and oral hygiene instruments can all be sources of virus exposure if they are not adequately sterilized.
Tattoos and body piercings can be a source of transmission of HCV if the instruments have been used on someone with HCV and have not been adequately sterilized. Personal items such as razors, manicuring scissors, pedicure equipment, and toothbrushes and dental floss, cancer sores and cold sores may become contaminated with blood. Any issue that produces bleeding can be the cause of spread of HCV from person to person.
HCV can be passed from the mother to the neonate (vertical transmission) infrequently during the delivery process. In mothers who are HCV RNA positive at the time of delivery the risk of transmission is six out of 100 deliveries and among women who are both HIV (human immunodeficiency virus) and HCV positive during delivery the transmission will be approximately 25 out of 100.
Approximately 60 percent of hepatitis C viral infection comes from injection drug use, 15 percent from sexual contact, 10 percent from blood transfusions before screening, 10 percent unknown, and 5 percent from other ( contamination, hemodialysis, health care work and passed from mother to neaonate during the birth process).
Acute and Chronic Hepatitis C
Acute hepatitis C refers to the first 6 months after infection with HCV although symptoms may appear within a day if infection was caused by any method of intravenous injection. Between 60% and 70% of people infected develop no symptoms during the acute phase unless infection was caused by direct access to the blood stream as crossing the blood brain barrier is then made up to 100 times easier. Main symptoms consist of general cold and flu like symptoms. In the minority of patients who experience acute phase symptoms, they are generally mild and nonspecific, and rarely lead to a specific diagnosis of hepatitis C. Symptoms of acute hepatitis C infection include decreased appetite, fatigue, abdominal pain, jaundice, itching, and flu-like symptoms.
The natural course of chronic hepatitis C varies considerably from one person to another. Although almost all people infected with HCV have evidence of inflammation on liver biopsy, the rate of progression of liver scarring (fibrosis) shows significant variability among individuals. Accurate estimates of the risk over time are difficult to establish because of the limited time that tests for this virus have been available.
Factors that have been reported to influence the rate of HCV disease progression include age (increasing age associated with more rapid progression), gender (males have more rapid disease progression than females), alcohol consumption (associated with an increased rate of disease progression), HIV co-infection (associated with a markedly increased rate of disease progression), and fatty liver (the presence of fat in liver cells has been associated with an increased rate of disease progression).
Symptoms specifically suggestive of liver disease are typically absent until substantial scarring of the liver has occurred. However, hepatitis C is a systemic disease and patients may experience a wide spectrum of clinical manifestations ranging from an absence of symptoms to a more symptomatic illness prior to the development of advanced liver disease. Generalized signs and symptoms associated with chronic hepatitis C include fatigue, flu-like symptoms, joint pains, itching, sleep disturbances, appetite changes, nausea, and depression.
Once chronic hepatitis C has progressed to cirrhosis, signs and symptoms may appear that are generally caused by either decreased liver function or increased pressure in the liver circulation, a condition known as portal hypertension. Possible signs and symptoms of liver cirrhosis include ascites (accumulation of fluid in the abdomen), bruising and bleeding tendency, varices (enlarged veins, especially in the stomach and esophagus which may unexpectedly rupture and cause uncontrolled bleeding), jaundice, and a syndrome of cognitive impairment known as hepatic encephalopathy. Hepatic encephalopathy is due to the accumulation of ammonia and other substances normally cleared by a healthy liver.
What Exactly is Hepatitis C?
Hepatitis C is one of the five known hepatitis viruses (A, B, C, D, E) caused by the hepatitis C virus which infects the liver. Sometimes a person will have no outward symptoms of having this infection, but once the virus is firmly established in the body the infection can lead to liver scarring (fibrosis) and then to advance scarring (cirrhosis). Cirrhosis may take many years to develop. Eventually there can be liver failure which could lead to the need for a liver transplant and/ or to liver cancer. The newly transplanted liver will then become subject to the hepatitis C virus if the virus is still active in a person.
Medical history can be a key to suspected chronic hepatitis C infection. Key factors would be history of IV drug use or inhaled substance use, a history of tattoos and/ or piercings, abnormal liver function tests and enzymes found during routine blood testing, unexplained symptoms, and infrequently during screenings for routine blood donation.
Hepatitis C is passed from person to person through blood contact. Acute hepatitis C denotes the first six months after infection. Symptoms are those of the common cold and flu with a decreased appetite, feeling tired, abdominal pain, jaundice (yellowing of the skin and whites of the eyes), and itching. Sixty to 70 percent of those infected will have no immediate symptoms unless the viral infection was caused by the direct entrance to the blood stream (sharing of needles with infected person).
The hepatitis C virus is usually detectable within one to three weeks after infection and antibodies will be present in the subsequent three to fifteen weeks after infection. Many people exposed to the hepatitis C virus will be able to automatically rid themselves of the virus during this acute phase.
Persistent infections are common and most of these patients develop chronic hepatitis C which by definition is the infection lasting more than six months. Again, chronic infection with the hepatitis C virus may produce no symptoms for the patient, although it is the leading cause of liver disease in the United States. The course of chronic infection can vary from person to person, but generally there will be an inflammation of the liver with eventual scarring. The amount of and timing of the scarring is variable.
If left untreated, one third of those infected will develop cirrhosis of the liver in less time than twenty years and another one third will take thirty years to progress to full cirrhosis. The remaining one third will develop cirrhosis so slowly that they will probably die before developing cirrhosis. Increasing age, alcohol consumption, and fatty liver (presence of fat cells in the liver) have all been associated with the progression of the disease. Symptoms of chronic infection may be joint pains, fatigue, flu-like symptoms, disturbances in sleep patterns, itching, depression, nausea, and alteration in appetite.
Chronic hepatitis C, which has progressed to cirrhosis, will present with the symptoms normally associated with liver disease. These would be due to increased pressure in the liver circulatory system (portal hypertension) and/or a decreased ability of the liver to function. Signs of liver cirrhosis are jaundice, accumulation of fluid in the abdomen (ascites), increased bruising and bleeding, enlarged veins in the stomach and esophagus which are apt to bleed (possibly to the extent of causing death due to abrupt blood loss), and hepatic encephalopathy which is caused by the accumulation of byproducts (ammonia) of normal food usage, but accompanied by the inability of the liver to filter out these harmful byproducts.
Co-infection with HCV and HIV occurs in approximately 35 percent of the patients in the U.S. Both diseases are blood- borne and can be present in related populations. The addition of HCV in a person with HIV will generally cause a more rapid progression of chronic hepatitis C to cirrhosis and then to liver failure. There are treatments for patients with both HIV and HCV infections.
Treatments
The scope of this article does not deal with the specifics of drug treatments. Your healthcare provider would be your best source of information on treatments. Currently treatments with interferon (pegylated interferon alpha) and ribavirin (anti-viral) are used, but there are ongoing studies and drug developments.
References
Crax, Antonio. Journal of Hepatology online February 28, http://www.jhep-elsevier.com/home.
Hendrik, Bill. Signs of Rise in Hepatitis C Cases Among Young. Accessed on May 12, 2011. http://www.medscape.com/viewarticle/742550
Loomba, R., M. M. Rivera, R. McBurney, Y. Park; V. Haynes-Williams, B. Rehermann; H. J. Alter,S. K. Herrine, T. J. Liang, J. H. Hoofnagle & T. Helle. The Natural History of Acute Hepatitis C: Clinical Presentation, Laboratory Findings and Treatment Outcomes. Posted: 05/05/2011; Alimentary Pharmacology & Therapeutics. 2011;33(5):559-565. © 2011 Blackwell Publishing

Carol graduated from Riverside White Cross School of Nursing in Columbus, Ohio and received her diploma as a registered nurse. She attended Bowling Green State University where she received a Bachelor of Arts Degree in History and Literature. She attended the University of Toledo, College of Nursing, and received a Master’s of Nursing Science Degree as an Educator.
She has traveled extensively, is a photographer, and writes on medical issues. Carol has three children RJ, Katherine, and Stephen – one daughter-in-law; Katie – two granddaughters; Isabella Marianna and Zoe Olivia – and one grandson, Alexander Paul. She also shares her life with her husband Gordon Duff, many cats, and two rescues.
ATTENTION READERS
We See The World From All Sides and Want YOU To Be Fully InformedIn fact, intentional disinformation is a disgraceful scourge in media today. So to assuage any possible errant incorrect information posted herein, we strongly encourage you to seek corroboration from other non-VT sources before forming an educated opinion.
About VT - Policies & Disclosures - Comment Policy




Comments are closed.