USA: The number of pregnant people who are getting vaccinated is steadily increasing amid the coronavirus current surge, but health experts say the modest improvement is not enough, as those who are expecting to continue to get critically ill or die from COVID-19.
The Covid in Pregnancy Study in Scotland shows the devastating consequences contracting COVID-19 in pregnancy can have for mothers and their babies and how crucial it is that pregnant women are vaccinated against the virus: https://t.co/fSAWPZB5Yb
— RoyalCollegeObsGyn (@RCObsGyn) January 14, 2022
The renewed concern comes following a large study published Thursday in “Nature Medicine” that shows unvaccinated pregnant people and their babies may suffer the worst consequences of the virus.
*New data* from 79,148 ppl giving birth in Scotland Mar 20 – Oct 21.
🦠 #COVID ⬆️ risk of stillbirth or neonatal death by ~4x, and preterm birth by ~2x
💉 #CovidVaccination protects against COVID and is not associated with poor #pregnancy outcomes. 1/https://t.co/VZikOYvI57 pic.twitter.com/LL5PdeLL2x
— Viki Male (@VikiLovesFACS) January 13, 2022
Researchers at the University of Edinburgh Usher Institute analyzed data collected by the COVID-19 in Pregnancy in Scotland study – a national cohort of women who were pregnant on, or became pregnant after, March 1, 2020. The database tracked nearly 145,000 pregnancies in 130,000 women from March 2020 to Oct. 2021.
CW: pregnancy and COVID
Omicron, for whatever reason, seems very bad for pregnant people. Doc friend’s doc friend analyzing data saying something about the clotting and embolisms omicron is becoming famous for. If pregnant: Vaccinate, boost, mask up, isolate.
— unfard (@unfard) January 6, 2022
The study found 98% of pregnant women admitted to critical care were unvaccinated. Researchers reported more than 450 perinatal deaths, when a baby dies in the womb or during the newborn period, all associated with unvaccinated pregnant women.
“The key take-home message that we’d love to get across is that the better way to protect mom and baby is vaccination at the earliest opportunity, and that can be done at any stage in pregnancy,” Aziz Sheikh, study co-author and professor at the University of Edinburgh said during a press briefing Thursday.
This needs to be highlighted again. Stark reality of Covid in pregnancy from the UK 230 women in ICU in delta wave May-October. 17 mothers and 4 babies tragically died. Only 0.4% of those admitted to ICU were double vaccinated. The vaccine offers a high level of protection. pic.twitter.com/bjxlzUXTt4
— Clare O’Connor (@drclareoconnor) January 4, 2022
The rate of perinatal mortality for women who gave birth within the study period was higher than the pandemic background rate at 22.6 per 1,000 births compared to 5.6.
Pregnancy + COVID = high risk for Covid complications and newborn deaths https://t.co/HFUwi0QGDw
— E. Rosalie (@NovelSci) January 14, 2022
The study also found 77% of the nearly 5,000 COVID-19 infections among pregnant women occurred in those who were unvaccinated. Health experts speculate this figure may be higher, as some of the vaccinated pregnant people seeking care may have been hospitalized for reasons other than COVID-19 but tested positive upon admission.
https://www.usatoday.com/story/news/health/2022/01/13/pregnant-unvaccinated-covid-baby-dangers/9185639002/
- Article
- Open Access
- Published:
SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland
Nature Medicine (2022)Cite this article
Abstract
Population-level data on COVID-19 vaccine uptake in pregnancy and SARS-CoV-2 infection outcomes are lacking. We describe COVID-19 vaccine uptake and SARS-CoV-2 infection in pregnant women in Scotland, using whole-population data from a national, prospective cohort. Between the start of a COVID-19 vaccine program in Scotland, on 8 December 2020 and 31 October 2021, 25,917 COVID-19 vaccinations were given to 18,457 pregnant women. Vaccine coverage was substantially lower in pregnant women than in the general female population of 18−44 years; 32.3% of women giving birth in October 2021 had two doses of vaccine compared to 77.4% in all women.
The extended perinatal mortality rate for women who gave birth within 28 d of a COVID-19 diagnosis was 22.6 per 1,000 births (95% CI 12.9−38.5; pandemic background rate 5.6 per 1,000 births; 452 out of 80,456; 95% CI 5.1−6.2). Overall, 77.4% (3,833 out of 4,950; 95% CI 76.2−78.6) of SARS-CoV-2 infections, 90.9% (748 out of 823; 95% CI 88.7−92.7) of SARS-CoV-2 associated with hospital admission and 98% (102 out of 104; 95% CI 92.5−99.7) of SARS-CoV-2 associated with critical care admission, as well as all baby deaths, occurred in pregnant women who were unvaccinated at the time of COVID-19 diagnosis. Addressing low vaccine uptake rates in pregnant women is imperative to protect the health of women and babies in the ongoing pandemic.
Main
Comprehensive whole-population data on COVID-19 vaccine uptake in pregnancy and SARS-CoV-2 infection rates and COVID-19 outcomes are lacking1. Such data are required to help guide decision-making by women, clinicians, and policymakers on measures to prevent and control COVID-19 in pregnancy, in particular, vaccination.
The first case of SARS-CoV-2 in Scotland was identified on 1 March 2020. Different SARS-CoV-2 variants have predominated in subsequent waves of infection, with wild type predominant initially, the Alpha variant dominant from January 2021, and the Delta variant dominant from May 2021. SARS-CoV-2 testing was initially restricted due to limited availability, with availability in the community for any symptomatic adult available from 18 May 2020. Although not uniformly implemented in all maternity units, routine SARS-CoV-2 testing of maternity admissions was instituted from 1 December 2020.
Pregnant women do not seem to be more susceptible to SARS-CoV-2 infection than non-pregnant women, but they are at higher risk of severe COVID-19 disease2,3,4. Compared to non-pregnant women of reproductive age, pregnant women with SARS-CoV-2 infection are more likely to be admitted to critical care, receive invasive ventilation and extracorporeal membrane oxygenation, and die2,3. COVID-19 in pregnancy is associated with an increased risk of pregnancy-specific complications pre-eclampsia, preterm birth, and stillbirth2,5,6,7,8,9,10.
Despite widespread recognition of potential vulnerability to COVID-19, pregnant women were excluded from pre-marketing clinical trials studying COVID-19 vaccines11,12. As a result, evidence to inform decision-making on vaccination was largely absent when vaccination programs started and recommendations on vaccination in pregnancy have varied over time as well as by country13. Post-marketing surveillance data suggest that COVID-19 vaccine effectiveness is broadly similar to that in non-pregnant individuals14,15. Data on the safety of vaccines in pregnancy comes from preclinical studies of COVID-19 vaccines in animals16, findings from women who had unanticipated pregnancies while participating in clinical trials17, and accumulating pharmacovigilance data18,19,20,21, all of which are reassuring regarding COVID-19 vaccine safety in pregnancy.
The COVID-19 vaccination program in Scotland commenced on 8 December 2020 and policies on the provision of COVID-19 vaccination to pregnant women evolved over time (Fig. 1). From 16 April 2021, the recommendation has been that women who are pregnant should be offered vaccination at the same time as non-pregnant women, based on their age and clinical risk group, and no pregnancy-specific pre-vaccination counseling is required.
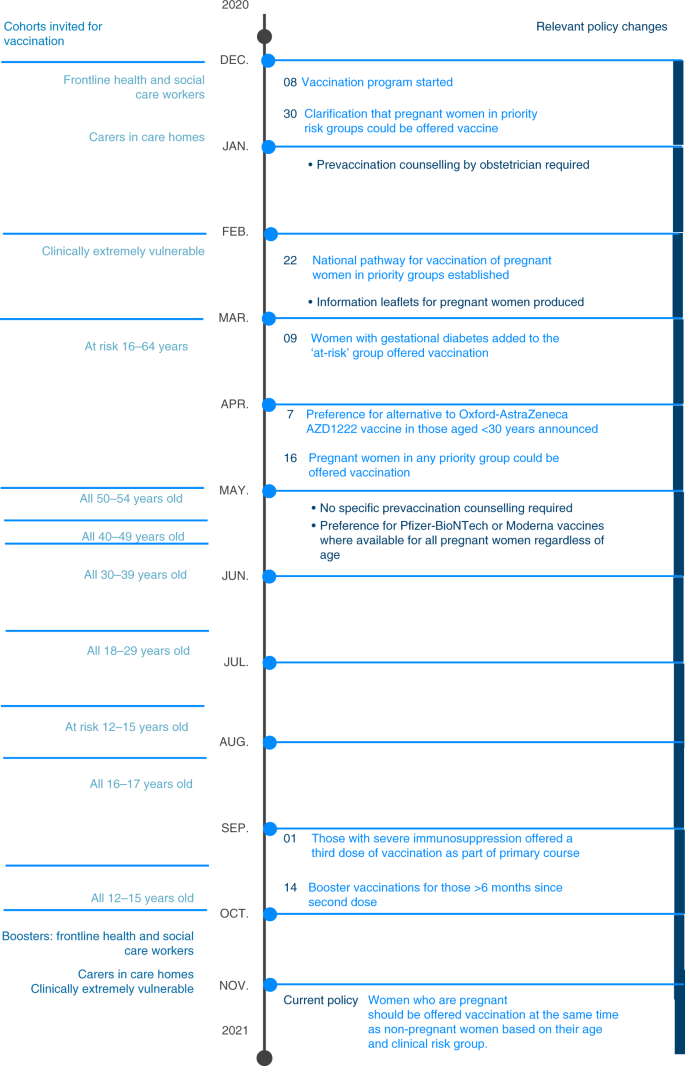
Summary of population cohorts invited for COVID-19 vaccination over time in Scotland from the start of the vaccination program on 8 December 2020 (left) and policy changes relevant to vaccination in pregnant women (right).
The COVID-19 in Pregnancy in Scotland (COPS) study (a sub-study of EAVE II (Early Pandemic Evaluation and Enhanced Surveillance of COVID-19)22,23) is a national, prospective dynamic cohort of all women who were pregnant on, or became pregnant after, 1 March 2020; linked to SARS-CoV-2 infection data and COVID-19 vaccination data24,25. The aims of this study were to use data from the COPS cohort to describe the uptake and coverage of COVID-19 vaccination in pregnant women; to describe the incidence of SARS-CoV-2 infection in pregnant women; to describe rates of hospital admission, critical care admission, preterm birth and extended perinatal mortality following SARS-CoV-2 infection in pregnancy; and to explore the effect of COVID-19 vaccination status on these post-infection outcomes.
Results
Cohort
We used the COPS database linked to records of COVID-19 vaccinations delivered and SARS-CoV-2 infections diagnosed up to and including 31 October 2021. This included data on a total of 145,424 pregnancies in 131,751 women. Overall, 144,548 (99.4%) of these pregnancy records (and 130,875, 99.3% of the women) had an associated unique community health index (CHI) number used for data linkage. Pregnancy records with no associated CHI number are likely to relate to duplicate records so were excluded from this analysis. Figure 2 describes the participants in the cohort. Overall, 117,190 pregnancies were complete, with 13,933 ending in early pregnancy loss (miscarriage, molar or ectopic pregnancy), 20,480 resulting in termination of pregnancy, 79,148 resulting in delivery and 3,629 having an unknown outcome. The deliveries resulted in 273 stillbirths and 80,183 live births, of which 179 resulted in neonatal death. Overall, 27,358 pregnancies were ongoing on 31 October 2021.
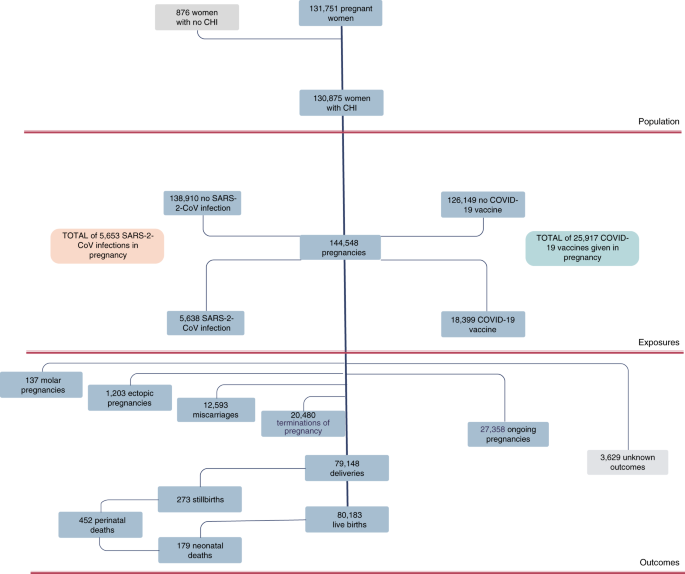
Flow chart summarizing participants in the COPS cohort. Counts for molar pregnancies, ectopic pregnancies, miscarriages, terminations and deliveries are numbers of pregnancies. Live births, stillbirths and neonatal deaths are numbers of babies.
Pregnancy data were linked with national data on confirmed SARS-CoV-2 infection and COVID-19 vaccination using CHI numbers. Overall, 99% of all the PCR with reverse transcription (RT−PCR) samples within the national testing database since the start of the pandemic, and 99.8% of all records for vaccinations given from the start of the program, have an associated CHI number.
Infection and vaccination in pregnancy were defined as infection diagnosed or vaccination given at any point from the date of conception (2 + 0 weeks gestation) to the date the pregnancy ends inclusive. The date of the first positive viral RT−PCR sample collection was taken as the date of onset of the first episode of COVID-19. Subsequent episodes were recorded if a positive viral RT−PCR sample was taken ≥90 d after a first positive sample.
To explore the impact of vaccination status on SARS-CoV-2 infection, women were grouped as follows: unvaccinated (no previous COVID-19 vaccination before the date of onset of COVID-19 or with one dose of vaccination ≤21 d before the date of onset); partially vaccinated (one dose of vaccination >21 d before the date of onset of COVID-19 or two doses of vaccination with the second dose administered ≤14 d before the date of onset); or fully vaccinated (two doses of vaccination with the second dose >14 d before the date of onset of COVID-19). We also report the number of third or booster doses given but have not included these in definitions of vaccination status, as third and booster doses in Scotland were only recommended from 14 and 20 September 2021, respectively.
COVID-19 vaccine coverage and uptake in pregnancy
From 1 December 2020 to 31 October 2021 a total of 25,917 COVID-19 vaccinations (12,518 (48%) first doses, 12,194 (47%) second doses and 1,205 (5%) third or booster doses) had been given in 18,399 pregnancies. A total of 9,905 (38.2%; 95% CI 37.6−38.8) vaccinations were given in the first trimester of pregnancy (at 2 + 0 to 13 + 6 weeks gestation); 9,317 (35.9%; 95% CI 35.4−36.5) in the second trimester (at 14 + 0 to 27 + 6 weeks gestation); and 6,695 (25.8%; 95% CI 25.3−26.4) in the third trimester (at 28 + 0 weeks gestation or over). Of the vaccinations given, 20,572 (79.4%; 95% CI 78.9−79.9) were Pfizer-BioNTech BNT162b2 messenger RNA vaccine; 3,224 (12.4%; 95% CI 12.0−12.8) were Moderna mRNA-1273 mRNA vaccine; and 2,121 (8.2%; 95% CI 7.9−8.5) were Oxford-AstraZeneca AZD1222 viral vector vaccine (given mainly early in the vaccine program to pregnant women with a clinical risk factor indicating vaccination).
We used two different metrics to describe vaccination in pregnancy, monthly uptake in women who were pregnant during the month and coverage (the proportion of women who, at the time of giving birth, had been vaccinated, whether vaccination was before or during pregnancy). Uptake and coverage data in the general female population of reproductive age (18−44 years) were provided for context, generated from data collected by Public Health Scotland26.
COVID-19 vaccine uptake among pregnant women each month was consistently lower than that in the general female population of reproductive age (Fig. 3a). Vaccine uptake was consistently lowest in younger (≤20 years) pregnant women and those living in the most deprived areas of Scotland (Fig. 3b,c).
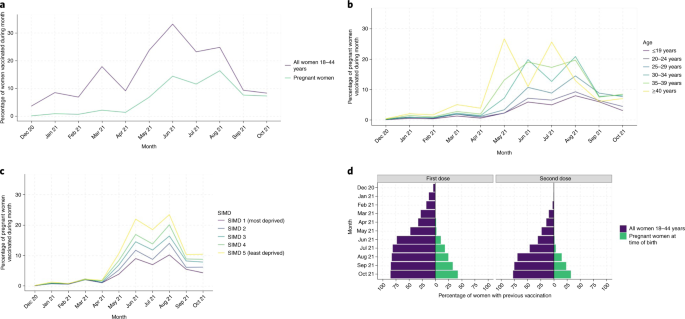
a, Monthly uptake of COVID-19 vaccination in all women 18−44 years and in pregnant women. b, Monthly uptake of COVID-19 vaccination in pregnant women by age group. c, Monthly uptake of COVID-19 vaccination in pregnant women by SIMD quintile. SIMD, Scottish Index Multiple Deprivation, with SIMD 5 being least deprived and 1 being most deprived. d, Vaccine coverage in the general female population in women age 18−44 years (purple) and percentage of pregnant women vaccinated before the time of birth (green). The numbers of women 18−44 years were derived from 2020 mid-year population estimates26.
COVID-19 vaccine coverage increased over time but has consistently been substantially lower among pregnant women than in the general female population of reproductive age (Fig. 3d). In October 2021, 4,064 women gave birth, of whom 1,738 (42.8%; 95% CI 41.2−44.3) had received any COVID-19 vaccination before delivery, with 1,311 (32.3%; 95% CI 30.8−33.7) of the women having received two primary doses of vaccination and 36 women (0.9%; 95% CI 0.6−1.2) having received a third or booster dose of vaccination. In contrast, by 31 October 2021, 84.7% (803,241 out of 947,984; 95% CI 84.7−84.8) of women aged 18–44 years in the general population had received any vaccination, 77.4% had received two doses (733,942 out of 947,984; 95% CI 77.3−77.5) and 7.0% had received a third dose or booster dose (66,001 out of 947,984; 95% CI 6.9−7.0).
SARS-CoV-2 outcomes in vaccinated and unvaccinated pregnant women
Between 1 March 2020 and 31 October 2021, there were 5,653 confirmed SARS-CoV-2 infections in pregnancy. Overall, rates of SARS-CoV-2 infection in pregnancy showed similar patterns to those in the general female population of reproductive age, with peaks of infection in October 2020, January 2021, and September 2021 (Fig. 4a). SARS-CoV-2 infection rates have been consistently highest in pregnant women living in the most deprived areas and in younger, compared to older, pregnant women (Fig. 4b,c).
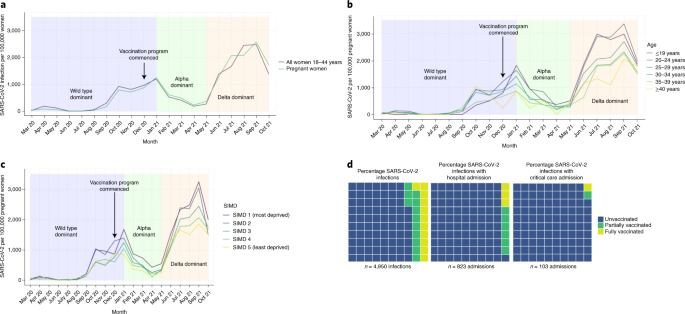
a, SARS-CoV-2 in all women 18−44 years per 100,000 women and in pregnant women. b, Monthly rates of SARS-CoV-2 per 100,000 pregnant women by age group c, Monthly rates of SARS-CoV-2 per 100,000 pregnant women by SIMD. d, Percentage of cases of SARS-CoV-2 infection in pregnancy occurring 1 December 2020 to 31 October 2021 inclusive, cases with associated hospital admission and cases with associated critical care admission, by vaccination status at the date of onset of COVID-19. Unvaccinated is defined as no COVID-19 vaccination before the date of onset of COVID-19 or one dose of vaccination ≤21 d previously in line with standard definitions used by Public Health Scotland.
Early in the pandemic, it is highly likely that there was an under-ascertainment of cases of SARS-CoV-2 infection due to limited test availability and testing capacity (Fig. 4a). Restricting the COPS cohort to only data from 1 December 2020 onward (the date that routine SARS-CoV-2 testing was recommended for all admissions to maternity care and the COVID-19 vaccination program started in Scotland) reduces the size of the cohort, but allows a more comparable estimation of rates of severe outcomes (hospital admission, critical care admission and perinatal mortality) associated with SARS-CoV-2 infection in vaccinated and unvaccinated women. From 1 December 2020 onward, the COPS database included linked data on a total of 91,183 pregnancies in 87,694 women.
There were 4,950 confirmed SARS-CoV-2 infections in pregnancy from 1 December 2020. SARS-CoV-2 infections were relatively evenly spread throughout pregnancy (1,543 (31.2%; 95% CI 29.9−32.5) diagnosed in the first trimester of pregnancy; 1,850 (37.4%; 95% CI 36.0−38.7) in the second trimester; and 1,557 (31.5%; 95% CI 30.2−32.8) in the third trimester).
Overall, 823 of the 4,950 SARS-CoV-2 infections in pregnancy from 1 December 2020 onward (16.6%; 95% CI 15.6−17.7) were associated with any hospital admission (date of onset of infection occurred during hospital admission or within 14 d before admission) and 104 SARS-CoV-2 infections in pregnancy (2.1%; 95% CI 1.7−2.6) were associated with a critical care admission (date of onset of infection occurred during a critical care admission or within 21 d before admission). In first trimester SARS-CoV-2 infections, 6.7% (103 out of 1,543; 95% CI 5.5−8.1) were associated with any hospital admission, compared to 10.7% (198 out of 1,850 cases; 95% CI 9.3−12.2) of those in the second trimester and 33.5% (522 out of 1,557; 95% CI 31.2−35.9) of those in the third trimester. No (0 out of 1,543 cases; 95% CI 0−0.3) SARS-CoV-2 infections in the first trimester were associated with critical care admission, compared to 2.0% (37 out of 1,850 cases; 95% CI 1.4−2.8) of those in the second trimester and 4.3% (67 out of 1,557; 95% CI 3.4−5.5) of those in the third trimester.
From 1 December 2020 onward, 77.4% of SARS-CoV-2 infections in pregnancy (3,833 out of 4,950; 95% CI 76.2−78.6) occurred in women who were unvaccinated at the date of onset of infection, with 11.5% (567 out of 4,950; 95% CI 10.6−12.4) in partially vaccinated women and 11.1% (550 out of 4,950; 95% CI 10.3−12.0) in fully vaccinated women.
Of the SARS-CoV-2 infections in pregnancy that occurred in unvaccinated women, 19.5% (748 out of 3,833; 95% CI 18.3−20.8) were associated with hospital admission, compared to 8.3% (47 out of 567; 95% CI 6.2−10.9) of those in partially vaccinated women and 5.1% (28 out of 550; 95% CI 3.5−7.4) of those in fully vaccinated women. A total of 2.7% (102 out of 3,833; 95% CI 2.2−3.2) of the SARS-CoV-2 infections in pregnancy that occurred in unvaccinated women were associated with a critical care admission, compared to 0.2% (1 out of 567; 95% CI 0.01−1.1) of those in partially vaccinated women and 0.2% (1 out of 550 cases; 95% CI 0.01−1.2) of those in fully vaccinated women. This means that while 77.4% (3,833 out of 4,950; 95% CI 76.2−78.6) of SARS-CoV-2 infections in pregnancy occurred in unvaccinated women, 90.9% (748 out of 823; 95% CI 88.7−92.7) of infections associated with hospital admission and 98.1% (102 out of 104; 95% CI 92.5−99.7) of infections associated with critical care admission, were in unvaccinated women (Fig. 4d). To date, there has been one maternal death following SARS-CoV-2 infection in pregnancy in Scotland.
A total of 2,364 babies have been born to women who had SARS-CoV-2 infection in pregnancy between 1 December 2020 and 31 October 2021. Of these, 2,353 were live births, of which 241 were preterm births (<37 weeks gestation; preterm birth rate 10.2%; 95% CI 9.1−11.6). Overall, 610 of the live births and 101 of the preterm births occurred within 28 d of the date of onset of the mother’s SARS-CoV-2 infection, giving a preterm birth rate among babies born within 28 d of SARS-CoV-2 infection of 16.6% (95% CI 13.7−19.8).
Of the 2,364 total births, 11 were stillbirths (deaths in utero ≥ 24 weeks gestation) and eight live births resulted in neonatal deaths (death within 28 d of birth), giving an extended perinatal mortality rate of 8.0 per 1,000 births following SARS-CoV-2 infection at any point in pregnancy (19 out of 2,364; 95% CI 5.0−12.8). Ten of the stillbirths and four neonatal deaths occurred in babies born within 28 d of the onset of maternal infection, giving an extended perinatal mortality rate of 22.6 per 1,000 births (14 out of 620, 95% 12.9−38.5) in this population. All perinatal deaths following SARS-CoV-2 infection in pregnancy occurred in women who were unvaccinated at the time of SARS-CoV-2 infection. We do not have access to detailed clinical records to assess whether COVID-19 directly or indirectly contributed to the preterm births and deaths seen following maternal infection.
For comparison, the background preterm birth rate during the pandemic (from 1 March 2020 to 31 October 2021) was 8.0% (6,381 out of 80,183 live births; 95% CI 7.8−8.1) and the extended perinatal mortality rate was 5.6 per 1,000 births (452 out of 80,456 total births; 95% CI 5.1−6.2). When restricted to babies born to women with no confirmed SARS-CoV-2 infection during pregnancy the preterm birth rate was 7.9% (6,083 out of 77,209 live births; 95% CI 7.7−8.1) and the extended perinatal mortality was 5.6 per 1,000 births (432 out of 77,470 total births; 95% CI 5.1−6.1). These preterm and perinatal mortality rates are shown in Fig. 5, along with the preterm birth and extended perinatal mortality rates in women who received the COVID-19 vaccine in pregnancy (preterm birth rate of 8.6% (495 out of 5,752 live births in women who received COVID-19 vaccination in pregnancy; 95% CI 7.9−9.4) and 8.2% (134 out of 1,632 live births within 28 d of COVID-19 vaccination in pregnancy; 95% CI 7.0−9.6); and extended perinatal mortality of 4.3 per 1,000 births (25 out of 5,766 total births in women who received COVID-19 vaccination in pregnancy; 95% CI 2.9−6.4) and 4.3 per 1,000 births (7 out of 1,635 births within 28 d of COVID-19 vaccination; 95% CI 1.9−9.2)).
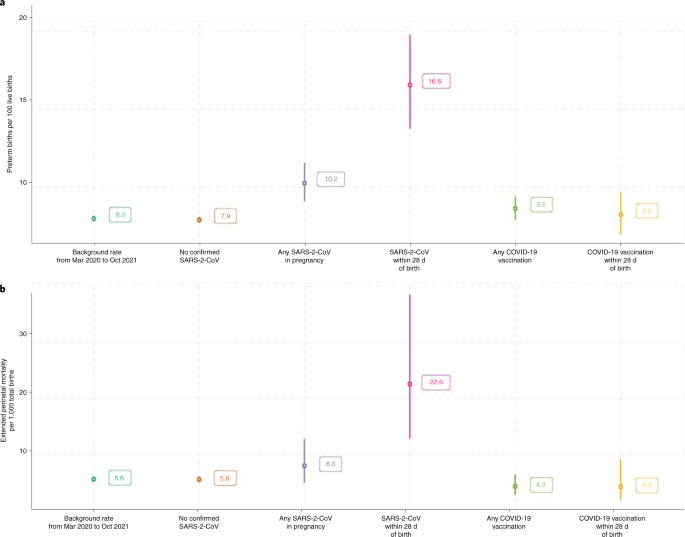
a,b, Preterm birth (<37 weeks gestation) rate per 100 live births (a) and extended perinatal mortality rates (b) (stillbirths (death in utero ≥24 weeks gestation) and neonatal deaths within 28 d of birth per 1,000 total births) in different cohorts during the pandemic. Background rate is the rate for all babies born during the pandemic period (1 March 2020 to 31 October 2021); no confirmed SARS-CoV-2 is the rate for babies born during the pandemic period (1 March 2020 to 31 October 2021) to women with no confirmed SARS-CoV-2 infection during pregnancy; any SARS-CoV-2 is the rate for babies born to women who had confirmed SARS-CoV-2 during their pregnancy 1 December 2020 to 31 October 2021; SARS-CoV-2 within 28 d of birth is the rate for babies born to women who had confirmed SARS-CoV-2 during their pregnancy 1 December 2020 to 31 October 2021, restricted to babies born within 28 d of the date of onset of maternal infection; Any COVID-19 vaccination is the rate for babies born to women who had COVID-19 vaccination during their pregnancy 1 December 2020 to 31 October 2021; COVID-19 vaccination within 28 d of birth is the rate for babies born to women who had COVID-19 vaccination during their pregnancy 1 December 2020 to 31 October 2021, restricted to babies born within 28 d of the date of maternal vaccination.
Discussion
These population data provide new national evidence of low levels of vaccine uptake in pregnancy in Scotland, at a time when the Delta variant dominated, with only 32.3% of pregnant women giving birth in October having had two doses of the vaccine. Rates were lowest in younger women and populations who lived in the most deprived areas. SARS-CoV-2 infection rates in pregnancy closely mirrored those in the general population throughout the pandemic, when different SARS-CoV-2 variants predominated in Scotland (wild type initially, Alpha dominant from January 2021, and Delta dominant from May 2021). We found that severe complications known to be associated with COVID-19 in pregnancy (critical care admission and perinatal mortality) were more common in women who were unvaccinated at the time of COVID-19 diagnosis than in vaccinated pregnant women. Our data support the importance of women being vaccinated in pregnancy to prevent adverse outcomes associated with COVID-19. For extended perinatal mortality, for example, we find substantially elevated rates among women who had SARS-CoV-2 within 28 d of birth; conversely, for women who had COVID-19 vaccination, extended perinatal mortality rates were similar to background rates and among women with no confirmed SARS-CoV-2.
Although surveillance studies, which have mainly been based on women admitted to hospital, have suggested that pregnant women are at the highest risk of severe COVID-19 disease in the third trimester9, these Scottish population data, capturing all virologically confirmed infections in a setting where testing has been widely available in the hospital and the community, show that SARS-CoV-2 infections were relatively evenly spread throughout pregnancy. However, in line with findings from other studies, SARS-CoV-2 associated with hospital and critical care admission was more common as pregnancy progressed4,9.
A strength of this study is that it used population data with high data completeness. Another strength is that the data describe changes in vaccine uptake over time, with most contemporary data available included. A caveat is that due to source data latency, the most recent 3 months’ pregnancy data may be less complete (there may be some under-ascertainment of the most recent pregnancies and end of pregnancy outcomes). A limitation of our study is that the data presented are descriptive and we have not adjusted for the potential confounding influence of demographics, obstetric or medical conditions. A fully adjusted analysis of all pregnancy outcomes (including early pregnancy outcomes) is planned27 when a greater number of end of pregnancy events have accumulated to ensure sufficient power, with appropriate historic comparison groups included28. Another limitation of our study is that we were unable to differentiate between hospital and critical care admissions due to SARS-CoV-2 infection from admissions for obstetric care with coincidental SARS-CoV-2 infection. SARS-CoV-2 infection in pregnancy may require admission in its own right for COVID-19 treatment; may trigger obstetric complications that require admission for maternity care or critical care (for example pre-eclampsia or delivery) or maybe an incidental finding on admission. Due to this complexity, routine population data coding was not sufficiently detailed to identify coincidental infections. Nevertheless, a comparison of hospital and critical care admissions within 28 d of SARS-CoV-2 infection, to those within 28 d of COVID-19 vaccination show different patterns (Fig. 6). Given the established safety profile of vaccinations18,19,20,21, we would anticipate that post-vaccination admissions are likely to be predominantly for obstetric indications. The higher levels of second and third-trimester hospital and critical care admissions following SARS-CoV-2 infections compared to vaccinations suggests that management of COVID-19 or its obstetric sequelae is the most likely reason for excess admissions.
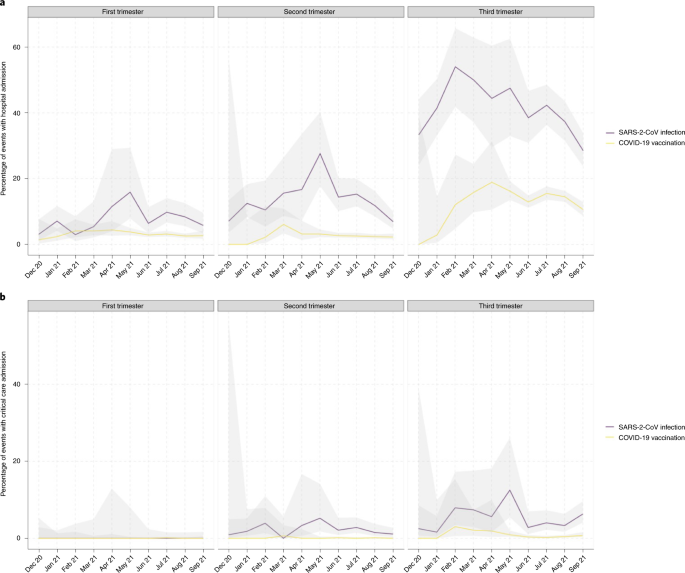
a, Percentage of cases of SARS-CoV-2 infections in pregnancy associated with hospital admission (defined as hospital admission ≤14 d after the date of diagnosis of SARS-2-CoV infection or if the date of diagnosis occurred at any point during a hospital admission) and COVID-19 vaccinations in pregnancy associated with hospital admission (defined as hospital admission ≤14 d after the date of COVID-19 vaccination) occurring 1 December 2020 to 30 September 2021. b, Percentage of SARS-CoV-2 infections in pregnancy associated with critical care admission (defined as critical care admission ≤21 d after the date of diagnosis of SARS-CoV-2 infection or if the date of diagnosis occurred at any point during a critical care admission) and COVID-19 vaccinations in pregnancy associated with critical care admission (defined hospital admission ≤21 d after the date of COVID-19 vaccination) occurring 1 December 2020 to 30 September 2021. Definitions are as per Public Health Scotland standards for associated hospital admission and critical care admission. Data are restricted to infections and vaccinations occurring up to 30 September 2021 due to incomplete follow-up times.
Our findings emphasize the need for continued efforts to increase vaccination uptake in pregnant women, especially in younger and more deprived populations29. The percentage of pregnant women vaccinated each month has declined since August 2021, reflecting the rollout of the vaccination program and the likelihood that an increasing proportion of women entering pregnancy are fully vaccinated. However, vaccine coverage, although increasing, remains low, with only a minority of pregnant women fully vaccinated by the time of delivery. Vaccine hesitancy in pregnancy thus requires addressing, especially in light of new recommendations for booster vaccination administration 3 months after the initial vaccination course to help protect against new variants such as Omicron30. Low levels of vaccine uptake in Scotland are likely to be representative of those in the United Kingdom and other high-income countries31 (Public Health Wales, personal communication). Addressing low vaccine uptake in pregnant women is imperative to protect the health of women and babies.
Methods
Ethics and data governance
COPS is a sub-study of EAVE II, using unconsented data that is covered by National Research Ethics Service Committee, South East Scotland 02 approval reference REC 12/SS/0201: SA 2. COPS has been approved by the Public Benefit and Privacy Panel approval reference 2021-0116. Public Health Scotland and the Chief Medical Officer for Scotland are both (independent) data controllers for the national Abortion Act Scotland (AAS) database of termination of pregnancy notifications, thus the Chief Medical Officer has been informed of the use of AAS records. All data were housed within a secure trusted research environment within Public Health Scotland and accessed only by approved researchers.
Study design and population
COPS is a prospective dynamic pregnancy cohort, identifying all ongoing and completed pregnancies in Scotland, United Kingdom, since 1 March 2020 (ref. 24). In this manuscript, we used the COPS database as updated in mid-November 2021 linked to records of COVID-19 vaccinations delivered and SARS-CoV-2 infections diagnosed up to and including 31 October 2021. Further detail on the datasets used is in the published protocol24. The COPS data dictionary is available online28. Data collection and analysis were performed in R v.3.6.1.
Maternity data sources and linkage
Ongoing pregnancies were identified using antenatal booking appointment data. Completed pregnancies were identified using multiple sources, specifically general practitioner records, general acute hospital discharge records, Scottish Morbidity Record (SMR) 01; maternity hospital discharge records, SMR 02; notification of termination data as governed by AAS; National Records of Scotland (NRS) statutory live birth registrations; NHS Scotland live births; and NRS statutory stillbirth registrations. These datasets capture miscarriage, molar pregnancy, or ectopic pregnancy requiring any general practitioner or hospital-based care, termination of pregnancy, live birth, or a stillbirth.
The CHI number is a unique patient identifier used across all health records in Scotland, enabling the integration of healthcare data. All source data incorporated into COPS were subject to a CHI-seeding process in which reported CHIs are reconciled to a contemporaneous unique patient identifier to ensure accurate linkage across sources.
Where multiple records within a data source pertained to the same woman, records were subject to event resolution, in which an iterative grouping procedure assigned records occurring within 83 d (less than 12 weeks) to a single healthcare event with its own universally unique identifier. The estimated date of conception was used to resolve records to a single pregnancy with a single universally unique identifier when gestation information was available and multiple records within a data source pertained to the same woman. Following event resolution, records from each individual data source were linked together to create a comprehensive record for each pregnancy and birth.
The COPS cohort is updated monthly and although source data latency means there is some instability in data for the most recent months, data are generally complete for conceptions and end of pregnancy events occurring up to 3 months previously.
National resources for SARS-CoV-2 infection data and COVID-19 vaccination data were incorporated into the study using CHI linkage.
SARS-CoV-2 infection and COVID-19 vaccination
Infection and vaccination in pregnancy were defined as infection diagnosed or vaccination is given, at any point from the date of conception (2 + 0 weeks gestation) to the date the pregnancy ends inclusive (censoring infections and vaccinations occurring at 44 + 0 weeks gestation or over as it is very likely that these women have completed their pregnancy, but the end of pregnancy record has not yet been received by Public Health Scotland). The date of the first positive viral RT−PCR sample collection was taken as the date of onset of the first episode of COVID-19. Subsequent episodes were recorded if a positive viral RT−PCR sample was taken ≥90 d after a first positive sample. Lateral flow test results were not considered. Anyone in Scotland having a positive lateral flow test is advised to have a follow-up RT–PCR test to confirm COVID-19.
Vaccination status was defined as unvaccinated (no previous COVID-19 vaccination before the date of onset of COVID-19 or with one dose of vaccination ≤21 d before the date of onset), partially vaccinated (one dose of vaccination >21 d before the date of onset of COVID-19 or two doses of vaccination with the second dose ≤14 d before the date of onset) or fully vaccinated (two doses of vaccination with the second dose >14 d before the date of onset of COVID-19).
Monthly vaccine uptake was calculated as the number of pregnant women vaccinated during the month divided by the number of women with ongoing pregnancies at the start of the month of interest. Coverage of vaccination at delivery was calculated as the proportion of women who, at the time of giving birth, have been vaccinated, whether vaccination was before or during pregnancy. Uptake in the general female population of reproductive age (18−44 years) was calculated as the number of women 18−44 years of age vaccinated during the month divided by the total number of women 18−44 years of age. Coverage in the general female population of reproductive age (18−44 years) was calculated as the cumulative number of women 18−44 years of age vaccinated by the end of each month divided by the total number of women 18−44 years of age. The numbers of women 18−44 years were derived from 2020 mid-year population estimates26. Although pregnant women 11−55 years of age were included in the COPS cohort, the comparator group was restricted to women 18−44 years. This is the Public Health Scotland standard definition of women of reproductive age and helps avoid bias in comparisons that could result from very low numbers of pregnancies at the extremes of reproductive age.
Hospital and critical care admission data
National hospital discharge records were linked to pregnancy SARS-CoV-2 RT−PCR testing data to identify women who were admitted to the hospital around the time of infection. Admissions to general acute units (SMR 01) and maternity units (SMR 02) were included. SARS-CoV-2 infection was defined as associated with a hospital admission if the woman was admitted to hospital ≤14 d after the date of onset of COVID-19 or if the date of onset occurred at any point during hospital admission (as per Public Health Scotland standard definition). National critical care discharge records from the Scottish Intensive Care Society Audit Group were used to identify women who were admitted to critical care. Completed admissions to all intensive care units and general (non-obstetric) high-dependency units across Scotland were included. Completed admissions to the seven obstetric high-dependency units that contribute data to the Scottish Intensive Care Society Audit Group (collectively covering around 60% of deliveries in Scotland) were also included. SARS-CoV-2 infection was defined as associated with a critical care admission if the woman was admitted to critical care ≤21 d after the date of onset of COVID-19 or if the date of onset occurred at any point during a critical care admission (as per Public Health Scotland standard definition).
Comparator data
Comparator data from the general population of women of reproductive age (taken as 18−44 years for these analyses) were obtained from Public Health Scotland Open data with mid-year population estimate denominators (2020)26.
Data quality and completeness
The national Scottish data used within this study undergo regular assessment and quality assurance with a high level of completeness and accuracy32,33. The CHI number was used to link the SARS-CoV-2 PCR testing data and COVID-19 vaccination records to the pregnancy records. Quality of linkage was assured by the testing, vaccination, and pregnancy records including complete and accurate information on individuals’ CHI numbers, as confirmed in the Results section.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data files of infections among pregnant women and the general population and vaccinations delivered to pregnant women and the general population are available at https://www.opendata.nhs.scot/organization/health_protection. Other personal data underlying this article cannot be shared publicly as they are sensitive. Public Health Scotland and the Chief Medical Officer for Scotland are the data holders for the data used in this study. Data are available to researchers for analysis after securing relevant permissions from the data holders. Inquiries regarding data availability should be directed to phs.edris@phs.scot.
Code availability
Metadata and code are available at https://github.com/Public-Health-Scotland/COPS-public.
References
- 1.
Razzaghi, H. et al. COVID-19 vaccination coverage among pregnant women during pregnancy – eight integrated health care organizations, United States, December 14, 2020–May 8, 2021. MMWR Morb. Mortal. Wkly Rep. 70, 895–899 (2021).
- 2.
Allotey, J. et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 370, m3320 (2020).
- 3.
Zambrano, L. D. et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status – United States, January 22–October 3, 2020. MMWR Morb. Mortal. Wkly Rep. 69, 1641–1647 (2020).
- 4.
Magnus, M.C. et al. Pregnancy and risk of COVID-19: a Norwegian registry-linkage study. BJOG https://doi.org/10.1111/1471-0528.16969 (2021).
- 5.
Villar, J. et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID Multinational Cohort Study. JAMA Pediatr. 175, 817–826 (2021).
- 6.
Papageorghiou, A. T. et al. Preeclampsia and COVID-19: results from the INTERCOVID prospective longitudinal study. Am. J. Obstet. Gynecol. 225, 289 (2021).
- 7.
Wei, S. Q., Bilodeau-Bertrand, M., Liu, S. & Auger, N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ 193, E540–E548 (2021).
- 8.
Knight, M. et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in the UK: national population-based cohort study. BMJ 369, m2107 (2020).
- 9.
Vousden, N. et al. The incidence, characteristics, and outcomes of pregnant women hospitalized with symptomatic and asymptomatic SARS-CoV-2 infection in the UK from March to September 2020: a national cohort study using the UK Obstetric Surveillance System (UKOSS). PLoS ONE 16, e0251123 (2021).
- 10.
Mullins, E. et al. Pregnancy and neonatal outcomes of COVID-19: coreporting of common outcomes from PAN-COVID and AAP-SONPM registries. Ultrasound Obstet. Gynecol. 57, 573–581 (2021).
- 11.
Luxi, N. et al. COVID-19 vaccination in pregnancy, pediatrics, immunocompromised patients, and persons with a history of allergy or prior SARS-CoV-2 infection: an overview of current recommendations and pre-and post-marketing evidence for vaccine efficacy and safety. Drug Saf. https://doi.org/10.1007/s40264-021-01131-6 (2021).
- 12.
Knight, M., Morris, R. K., Furniss, J. & Chappell, L. C. Include pregnant women in research-particularly COVID-19 research. BMJ 370, m3305 (2020).
- 13.
Johns Hopkins Berman Institute of Bioethics and the Johns Hopkins Center for Immunization Research. COVID-19 maternal immunization tracker (COMIT). https://www.comitglobal.org (2021).
- 14.
Goldshtein, I. et al. Association between BNT162b2 vaccination and incidence of SARS-CoV-2 infection in pregnant women. JAMA 326, 728–735 (2021).
- 15.
Gray, K. J. et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am. J. Obstet. Gynecol. 225, 303 (2021).
- 16.
Center for Disease Control (CDC). If you are pregnant, breastfeeding, or caring for young children. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Fpregnant-women-faq.html (2020).
- 17.
Hillson, K. et al. Fertility rates and birth outcomes after ChAdOx1 nCoV-19 (AZD1222) vaccination. Lancet 398, 1683–1684 (2021).
- 18.
Shimabukuro, T. T. et al. Preliminary findings of mRNA COVID-19 vaccine safety in pregnant persons. N. Engl. J. Med. 384, 2273–2282 (2021).
- 19.
Weinstock, T., Yoles, I., Sergienko, R. & Sheiner, E. Prenatal maternal COVID-19 vaccination, and pregnancy outcomes. Vaccine 39, 6037–6040 (2021).
- 20.
Theiler, R. N. et al. Pregnancy and birth outcomes after SARS-CoV-2 vaccination in pregnancy. Am. J. Obstet. Gynecol. MFM 3, 100467 (2021).
- 21.
Zauche, L. H. et al. Receipt of mRNA COVID-19 vaccines and risk of spontaneous abortion. N. Engl. J. Med. 385, 1533–1535 (2021).
- 22.
Simpson, C.R. et al. Early pandemic evaluation and enhanced surveillance of COVID-19 (EAVE II): protocol for an observational study using linked Scottish national data. BMJ Open 10, e039097 (2020).
- 23.
Mulholland, R. H. et al. Cohort profile: early pandemic evaluation and enhanced surveillance of COVID-19 (EAVE II) database. Int. J. Epidemiol. 50, 1064–1074 (2021).
- 24.
Stock, S. J. et al. COVID-19 in pregnancy in Scotland (COPS): protocol for an observational study using linked Scottish national data. BMJ Open 10, e042813 (2020).
- 25.
Stock S. J. et al. Cohort profile: the COVID-19 in pregnancy in Scotland (COPS) dynamic cohort of pregnant women to assess effects of viral and vaccine exposures on pregnancy. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyab243 (2022).
- 26.
Public Health Scotland. Open data. https://www.opendata.nhs.scot/dataset/covid-19-in-scotland (2021).
- 27.
Public Health Scotland. COPS-public Git Hub. https://github.com/Public-Health-Scotland/COPS-public (2021).
- 28.
Knight, M., Draper, E. & Kurinczuk, J. J. Misclassification bias and unnecessary anxiety. Am. J. Obstet. Gynecol. 225, 584 (2021).
- 29.
Iacobucci, G. COVID-19 and pregnancy: vaccine hesitancy and how to overcome it. BMJ 375, n2862 (2021).
- 30.
The Joint Committee on Vaccination and Immunisation (JCVI) advice on the UK vaccine response to the Omicron variant. https://www.gov.uk/government/publications/uk-vaccine-response-to-the-omicron-variant-jcvi-advice/jcvi-advice-on-the-uk-vaccine-response-to-the-omicron-variant (2021).
- 31.
UK Health Security Agency. Vaccine surveillance report. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1036047/Vaccine_surveillance_report_-_week_47.pdf (2021).
- 32.
NSS Information and Intelligence Assessment of SMR02 (Maternity Inpatient and Day Case) Data; Scotland 2017–2018. https://www.isdscotland.org/Products-and-Services/Data-Quality/docs/20191023-Assessment-of-SMR02-Data-Scotland-2017-2018.pdf (2019).
- 33.
Public Health Scotland. Data Quality Assurance Assessment of SMR01 (Acute Inpatient and Day Case) Data Scotland 2019–2020. https://www.isdscotland.org/Health-Topics/Hospital-Care/Publications/2012-05-08/Assessment-of-SMR01Data-2010-2011-ScotlandReport.pdf (2020).
Acknowledgments
We thank the EAVE II Patient Advisory Group and Sands charity for their support. COPS is a sub-study of EAVE II, which is funded by the Medical Research Council (MR/R008345/1) with the support of BREATHE, the Health Data Research Hub for Respiratory Health (MC_PC_19004; A.S.), which is funded through the UK Research and Innovation Industrial Strategy Challenge Fund and delivered through Health Data Research UK. Additional support has been provided through Public Health Scotland and Scottish Government DG Health and Social Care and the Data and Connectivity National Core Study, led by Health Data Research UK in partnership with the Office for National Statistics and funded by UK Research and Innovation. COPS has received additional funding from Tommy’s charity and support from Sands charity. S.J.S. is funded by a Wellcome Trust Clinical Career Development Fellowship (209560/Z/17/Z). S.V.K. acknowledges funding from an NRS Senior Clinical Fellowship (SCAF/15/02), the Medical Research Council (MC_UU_00022/2) and the Scottish Government Chief Scientist Office (SPHSU17). The funders had no role in the writing of the manuscript or the decision to submit it for publication. B.A. was supported by the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No. 813546, the Baily Thomas Charitable Fund TRUST/VC/AC/SG/469207686, the Data-Driven Innovation and the UK Economic and Social Research Council (ES/W001519/1) during the course of this work.
Ethics declarations
Competing interests
A.S. and C.R. are members of the Scottish Government’s COVID-19 Advisory Group. A.S. and C.R. are members of the New and Emerging Respiratory Virus Threats Advisory Group risk stratification subgroup. C.R. is a member of the Scientific Pandemic Influenza Group on Modeling. A.S. is a member of AstraZeneca’s Thrombotic Thrombocytopenic Advisory Group. All roles are unremunerated. R.W. and C.R. are employed by Public Health Scotland. S.J.S. has received research grants paid to the institution from Wellcome Trust, Scottish Chief Scientist Office, National Institute of Healthcare Research and Tommy’s during the course of this study. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Gianluca Trifirò, Deborah Money and Denise Jamieson for their contribution to the peer review of this work. Jennifer Sargent was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Additional information
Publisher’s Note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third-party material in this article are included in the article’s Creative Commons license unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Cite this article
Stock, S.J., Carruthers, J., Calvert, C. et al. SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland. Nat Med (2022). https://doi.org/10.1038/s41591-021-01666-2
- Received
- Accepted
- Published
- DOIhttps://doi.org/10.1038/s41591-021-01666-2
Subjects
- Epidemiology
- Viral infection
ATTENTION READERS
We See The World From All Sides and Want YOU To Be Fully InformedIn fact, intentional disinformation is a disgraceful scourge in media today. So to assuage any possible errant incorrect information posted herein, we strongly encourage you to seek corroboration from other non-VT sources before forming an educated opinion.
About VT - Policies & Disclosures - Comment Policy




So the extensive history of natural childbirth is now “out the window” with the bath water. The narrative and the minutia of this data is just another layer of deception coming from the “experts.”
Let it be simplified. Not a good time to get pregnant, but if you do, get the vaccine early.
The situation is, we are in a pandemic, and getting pregnant is not a wise choice.
The best intelligence is to not get pregnant at this time, as neither the covid or the vaccine is ideal for child birthing.
If you do get pregnant, You are the new people that go beyond. Every step is into the unknown. Best of luck. The survivors will be strong, and the dumb luck serves the rest,.
hu li o. Your question is oblique. But, most double blind drug tests involve the use of placebos or a non-vaccine vaccine. Why? Because there is no preconceived outcome of success or failure. The 90%+ efficacy reported from mRNA studies broke world records. The poor chumps who got the placebos probably all died.
One question;
is there any case, or any study dealing with covid vaccines, in which a “would be” normally vaccinated patient would be counseled to remain unvaccinated?
You are correct, Mihail, the actual numbers stated here imply something different from the headline. 77% we
e unvaccinated but the 23% vaccinated cases had other “conditions”. Maybe some of the 77% did too, huh? All drug studies try to prove preconceived outcomes or there would be no payday. This is not research or actual studies. Anyway, the general public will be kept totally confused. You are correct that the real proof is in actual cases, each of which is unique. But, that’s too much effort when sweeping generalizations are easier and people don’t question. Just ask the Fauc.
Another Mihail fail.
Comments are closed.